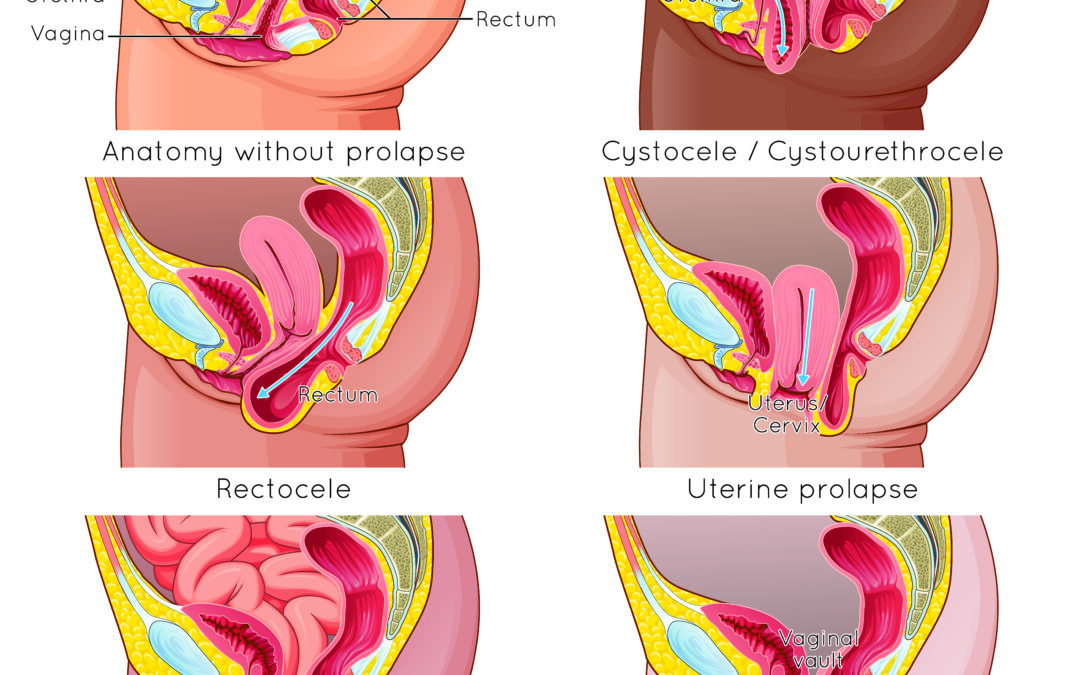
What is prolapse?
one or more pelvic organs can press into the vaginal wall and create prolapse.
If you’ve had babies or a hysterectomy, you may have heard of this
Types of pelvic organ prolapse (POP):
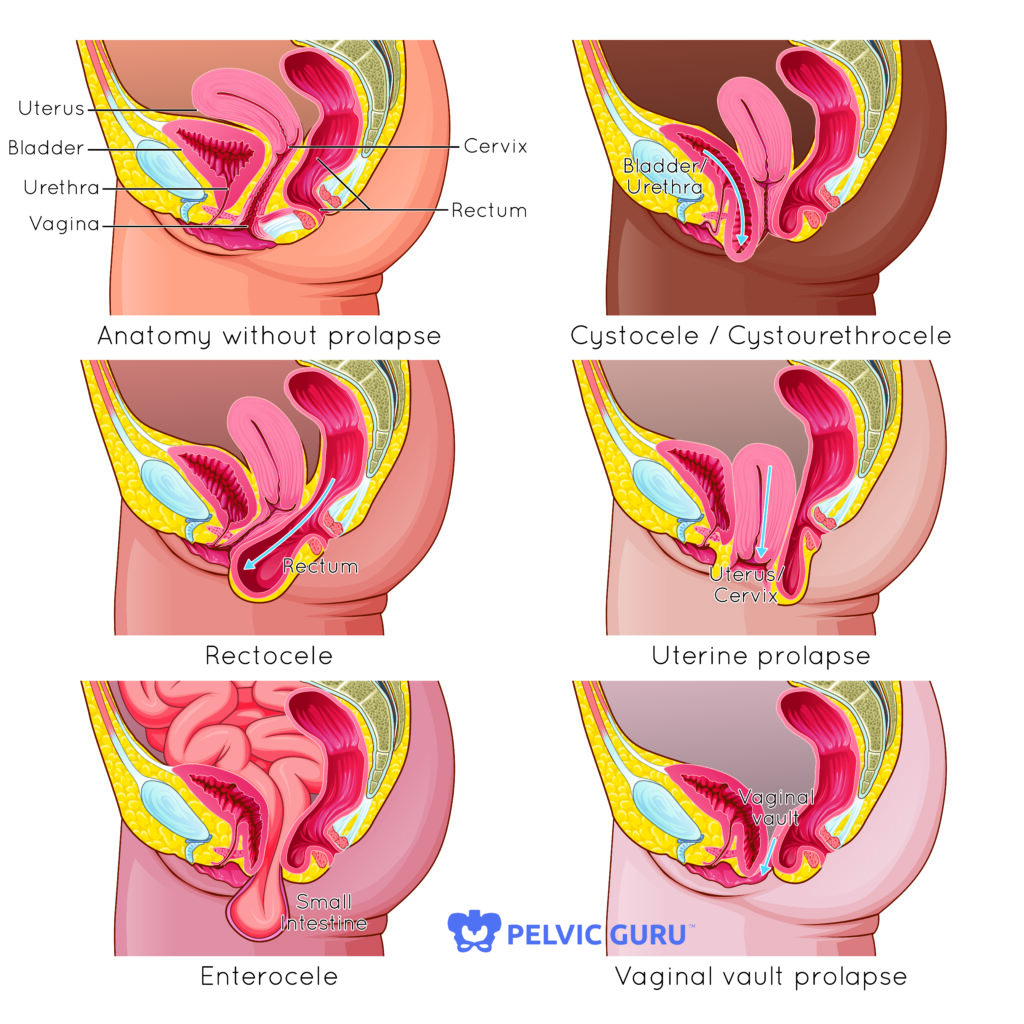
- Bladder (cystocele)
- Uterine prolapse
- Urethra (urethrocele)
- Small intestine (enterocele)
- Rectum (rectocele) – this is different from rectal prolapse, which is when the rectum is falling through the anus rather than the vaginal wall.
It sounds scary, but it can be a totally manageable condition!
Prolapse is generally caused by excessive intra-abdominal pressure, (genetics can play a role too). Usually, this happens in childbirth, but could be a result of improper movement patterns. For example, if you have constipation, frequently bearing down/straining to empty, you put a lot of pressure on your pelvic organs. When organs are softer than your poop, guess which is more likely to get pushed out? As a result, you may have a weakening of the tissues that support your pelvic organs. Pelvic floor tension may also contribute to prolapse because it can pull on the connective tissues and muscles that help with support.
About 1/3 of women will experience prolapse at some point in their lifetime*
Risk factors for prolapse:
- Vaginal childbirth (more with more births)
- Genetic ligament laxity or predisposition
- Frequent straining for constipation
- Straining during exercise
- Performing “kegels” incorrectly with bearing down vs lifting up
- Pelvic surgery (hysterectomy)
- Poor posturing and mechanics
- Weakness or lack of support in pelvic floor muscles
- Chronic tension in the abdomen or pelvic floor
Not all prolapse is symptomatic or even dysfunctional! You can have a prolapse and be fine! You may not even know! (Fun fact – I learned I have a mild prolapse during my first pelvic floor training course!)
Symptoms:
- Pressure or heaviness in your lower abdomen or pelvis
- A bulge feeling around the entrance of your vagina
- A pulling feeling in the groin area
- Incontinence (could also be dribbling after you’ve emptied your bladder)
- Feeling like you can’t fully empty your bladder
- Constipation or needing to apply pressure to the pelvic floor to empty bowel
- Typically, symptoms are worse towards the end of the day after you’ve been standing and walking, and better in the morning or after you’ve been laying down.
- You may have other issues such as back pain or painful intercourse. These vary depending on the severity and type of prolapse.
- You may not have symptoms at all!
Tips for Prolapse:
· Avoid straining in the bathroom! Try not to push when emptying your bowels or bladder. (If you are doing this, ask us about how we can help!)
· When exercising, be mindful of your breathing. Exhale as you are doing the hard part (contraction phase of the movement). Don’t know if you’re contracting properly? Ask us!
· Avoid things that create a lot of downward pressure into the pelvis without balancing that pressure with good support. See your Pelvic Physical Therapist for if/how you can do exercises correctly.
· Be mindful of your posture and body mechanics! Sitting slouched or hunched over puts extra pressure on the abdomen and can interfere with movement of our digestive system.
Think you might have prolapse? Get evaluated by a pelvic Physical Therapist! We can help you return to activity, relieve pain, and balance hormone and digestive health.
Check out our website for other ways Pelvic Physical Therapy can help!
*https://www.hopkinsmedicine.org/health/conditions-and-diseases/vaginal-prolapse